by Buck Institute
October 4, 2022 . Press Release
High Risk/High Reward Grant Funds Development of Smart Drug Delivery System to Treat Multiple Alzheimer’s Pathologies
The Buck’s $2.4 million Transformative Research Award is one of just nine in the nation.
Rather than attempting to treat the multiple pathologies of Alzheimer’s disease individually, as is the current practice, researchers in the Buck Institute’s Andersen lab have designed a smart cell-based delivery system (SmaCD) to treat them all at once. The National Institutes of Health considers the effort as high risk/high reward with the potential to change how we treat multiple diseases. It has awarded the lab with a $2.4 million Transformative Research Award to move the science forward, one of just nine awards made nationally.
 “Alzheimer’s is a complex disease with pathologies coming from at least three directions,” says Buck professor Julie Andersen, PhD. “Available drugs only target single pathologies, likely contributing to the dismal results we see in clinical trials for Alzheimer’s. The beauty of our system is that it delivers a combination therapy that addresses all of the pathologies in a targeted manner that also reduces the risk of side effects.”
“Alzheimer’s is a complex disease with pathologies coming from at least three directions,” says Buck professor Julie Andersen, PhD. “Available drugs only target single pathologies, likely contributing to the dismal results we see in clinical trials for Alzheimer’s. The beauty of our system is that it delivers a combination therapy that addresses all of the pathologies in a targeted manner that also reduces the risk of side effects.”
A smart cell-based delivery system – how it works
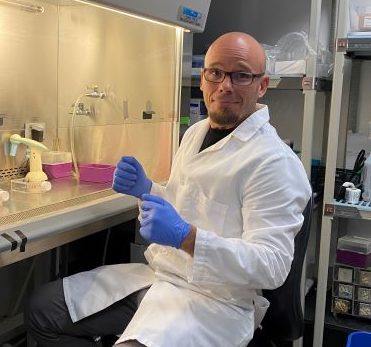 The SmaCD was designed by research scientist Chaska Walton, PhD, and it has a space age quality to it. Walton aims to turn immune cells into mobile biological drug factories that can “decide” when to release drugs at the site of pathology and, once cleared, can then move onto the next site of pathology. The SmaCD works with bio-synthesizable drugs, which are drugs based on amino acids that can be coded to churn out more of themselves as needed. In this case the combination therapy is based on two monoclonal antibodies: Aduhelm™(aducanumab-avwa), which is FDA approved to clear the amyloid plaques that are a hallmark of Alzheimer’s, and zagotenemab which failed a Phase II clinical trial aimed at clearing tau tangles, another feature of Alzheimer’s.
The SmaCD was designed by research scientist Chaska Walton, PhD, and it has a space age quality to it. Walton aims to turn immune cells into mobile biological drug factories that can “decide” when to release drugs at the site of pathology and, once cleared, can then move onto the next site of pathology. The SmaCD works with bio-synthesizable drugs, which are drugs based on amino acids that can be coded to churn out more of themselves as needed. In this case the combination therapy is based on two monoclonal antibodies: Aduhelm™(aducanumab-avwa), which is FDA approved to clear the amyloid plaques that are a hallmark of Alzheimer’s, and zagotenemab which failed a Phase II clinical trial aimed at clearing tau tangles, another feature of Alzheimer’s.
Walton’s project uses SmaCD to target the most afflicted regions of the brain with a combination therapy based on Aduhelm and zagotenemab. The goal is to activate microglia (which act as the first and main form of active immune defense in the central nervous system) to clear the amyloid plaques and disease-spreading tau, respectively, accompanied by an immuno-modulator to enhance the microglia’s ability to “eat” damaged cells, while suppressing inflammation at the same time. Walton’s Alzheimer’s project involves human and mouse cell cultures and in vivo studies in mice with mid- and late- stage disease. Highlighting SmaCD’s flexibility, Walton notes that the original project design is evolving as testing around Alzheimer’s antibodies is updated. He says the project could involve additional therapeutics that target other contributing factors to Alzheimer’s pathology such as variants in ApoE alleles and lipid transport.
At a basic level, Walton’s SmaCD is somewhat similar to CAR-T therapies which are providing breakthrough treatments for some forms of cancer. In those cases, specific immune cells are genetically altered and infused into patients to act as a “living drug” which recognizes cancer cells and destroys them. There is, however, a critical difference. “CAR-T’s are designed to kill and we don’t want to kill. We want to heal,” says Walton. “This platform is designed to act as a mini doctor that could go to targeted locations and deliver drugs in response to the environment and in different sequences as provoked by the pathology.”
“The path to using genetically-engineered cells to cure cancer was not easy,” says Walton. “However CAR-T has become a highly-used therapeutic in cancer. We think the timing is right. Alzheimer’s is now at the point at which cancer was prior to the development of CAR-T.”
The need for combination therapies that are safe
Given that amyloid beta and tau pathologies as well as brain inflammation and damage-related scarring (gliosis) are all harmful to the brain, Andersen thinks it’s unrealistic to expect that targeting a single pathological hallmark would improve cognition. She says the European Union-North American Clinical Trials in Alzheimer’s Disease Task Force (EU/US CTAD Task Force) is strongly encouraging the use of combination therapies. “In addition to targeting each specific pathology, our system would treat Alzheimer’s at the site of the pathology at various stages of the disease. The entire body would not be exposed to the drugs, giving us a way of avoiding the side effects which have been the bane of many attempts to bring drugs to the clinic.”
Walton, who comes from Spain, adds, “In my country, we have a saying ‘you’re killing flies with cannonballs’ and that’s been the problem with drugs created to treat Alzheimer’s and other conditions. We harm the body while attempting to cure the disease.”
Implications for big pharma, biotech and research on aging
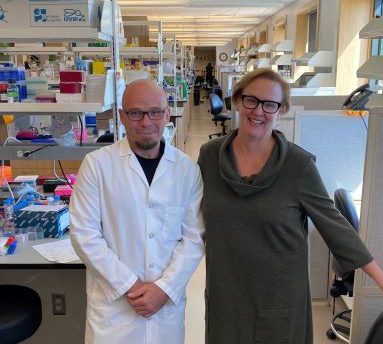 Both Walton and Andersen think SmaCD could give biotech and pharmaceutical companies that had failed clinical trials for Alzheimer’s another shot at success. “Their drugs worked really well in mice, but when they put them into humans they had to reduce dosages to avoid side effects, which affected efficacy. Now there’s a way they would be able to deliver their drugs only to the region where it’s needed,” says Andersen.
Both Walton and Andersen think SmaCD could give biotech and pharmaceutical companies that had failed clinical trials for Alzheimer’s another shot at success. “Their drugs worked really well in mice, but when they put them into humans they had to reduce dosages to avoid side effects, which affected efficacy. Now there’s a way they would be able to deliver their drugs only to the region where it’s needed,” says Andersen.
SmaCD can be edited to target organs, cells, and or extracellular proteins to locally deliver any bio-synthesizable drug, giving it wide applicability to treat numerous conditions, with aging among them. “Aging is so complex and it impacts our tissues in such diverse ways, I think it’s highly unlikely that we’re going to find a miracle drug that is going to touch all the molecular pathways in the right directions with the right intensities,” says Walton. “Imagine if we could target different organs that had different age-related pathologies and deliver drugs in a smart way. That would be a game-changer.”
Acknowledgement: This work is funded under NIH grant 1 R01 AG01081989
 About the NIH Common Fund: The NIH Common Fund encourages collaboration and supports a series of exceptionally high-impact, trans-NIH programs. Common Fund programs are managed by the Office of Strategic Coordination in the Division of Program Coordination, Planning, and Strategic Initiatives in the NIH Office of the Director in partnership with the NIH Institutes, Centers, and Offices. More information is available at the Common Fund website: https://commonfund.nih.gov.
About the NIH Common Fund: The NIH Common Fund encourages collaboration and supports a series of exceptionally high-impact, trans-NIH programs. Common Fund programs are managed by the Office of Strategic Coordination in the Division of Program Coordination, Planning, and Strategic Initiatives in the NIH Office of the Director in partnership with the NIH Institutes, Centers, and Offices. More information is available at the Common Fund website: https://commonfund.nih.gov.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
Science is showing that while chronological aging is inevitable, biological aging is malleable. There's a part of it that you can fight, and we are getting closer and closer to winning that fight.
Eric Verdin, MD, Buck Institute President and CEO