by Buck Institute
April 5, 2021 . BLOG
COVID-19: The Past, Present and Future of Pandemics
This is the 3rd blog in our series from MS Biology students from Dominican University. In this post, student authors Slesha Thapa, Jordan Tahquechi, Selma Takajjart, Sivan Brod-Abo, and Alyssa Gonzalez describe the history of pandemics and how we have beat them in the past. You can read the first blog, about vaccines, and the 2nd blog, about prevention.
By: Slesha Thapa, Jorden Tahquechi , Sivan Brodo-Abo, Selma Takajjart, Alyssa Gonzale;
Edited by Professor, Dr. Pankaj Kapahi
Pandemics: Through the Looking Glass
The history of pandemics is thought to date back to the BC era. But do you actually know what is considered a pandemic? The definition of a pandemic is “an outbreak of a disease that occurs over a wide geographic area (such as multiple countries or continents).” Pandemics originate from a virus or a bacterium, and spread rapidly throughout the world. However, before a disease is declared a pandemic, scientists usually ask these three questions: (1) How far has it spread? (2) How many people has it affected? and (3) Is it a new disease?
Of the major pandemics, Black Death, or the Bubonic Plague, is considered the most fatal pandemic in human history. Originating in rats and transmitted to humans by fleas infected with the bacterium Yersinia pestis, the Bubonic Plague led to about 200 million deaths. This pandemic wiped out between 30-50% of the population in Europe and it took more than 200 years for the population to recover. Another infamous pandemic was Smallpox, which resulted in approximately 56 million deaths. Smallpox was caused by the Variola major virus. In order to fight off smallpox, the first vaccine was developed, which you can read about in an earlier blog post.
Today of course we are facing a pandemic of our own: COVID-19. Although we know that COVID-19 is caused by the coronavirus SARS-CoV-2, we still do not know where exactly this disease came from, and how it spread to humans. This disease has already caused 1.8 million deaths, and that number will unfortunately continue to increase as we are still battling this pandemic.
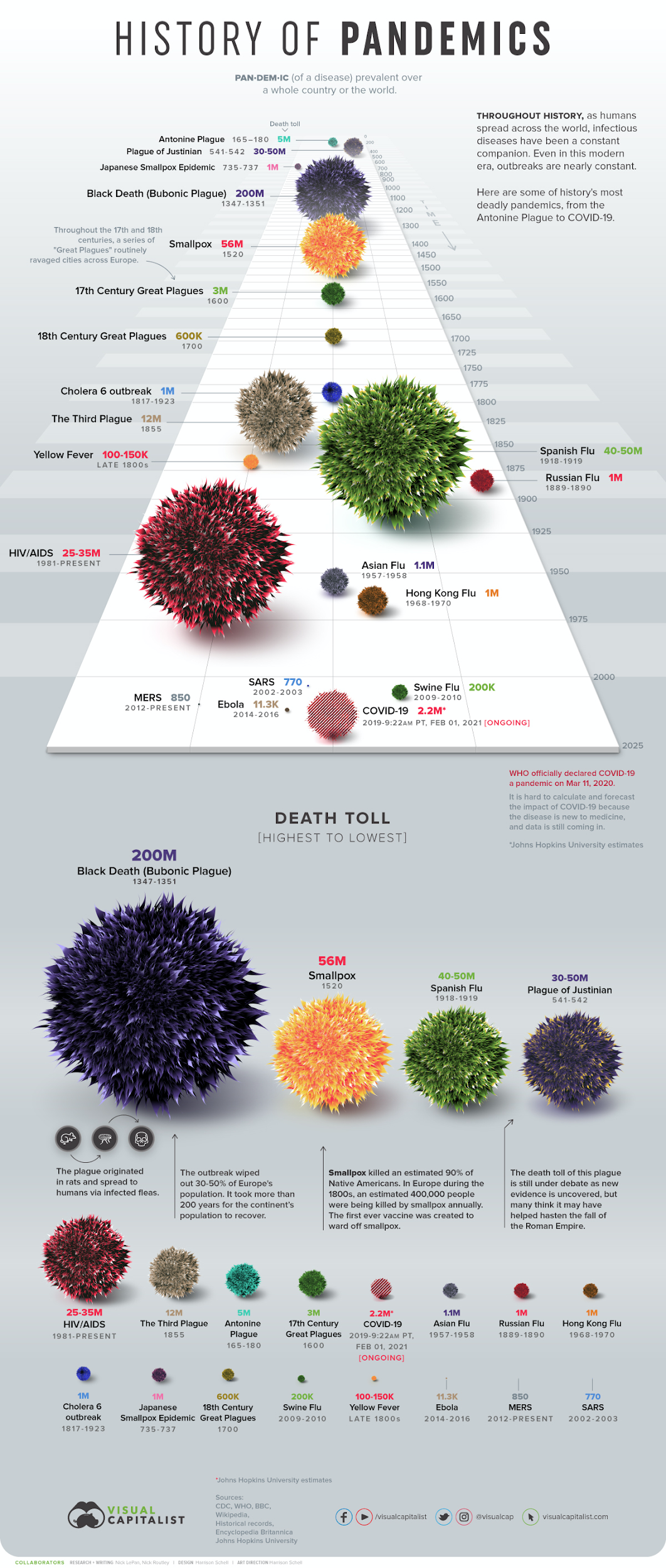
Timeline of the major pandemics that we have experienced throughout time.
Corona? Like the beer?
It is interesting to consider where pandemic names come from and who exactly names them. Contrary to some social media speculation at the beginning of the outbreak, there is no correlation between this virus and the beer Corona. COVID-19 was initially named 2019-nCoV by the World Health Organization (WHO) in January 2020. However, by February 2020, the WHO renamed this disease COVID-19 (CO-corona, VI-virus, D-disease, and 2019-19). On the same day the disease was renamed, the Coronavirus Study Group (CSG) suggested naming it severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). These two names are often used interchangeably, but one way to sum it up is that COVID-19 is the disease, SARS-CoV-2 is the name of the virus, just as AIDS is the disease caused by the HIV virus. The word “Corona” is defined as “a usually colored circle often seen around and close to a luminous body (such as the sun or moon)”. It is also the Spanish word for crown. This description resembles what the SARS-CoV-2 virus or the coronaviruses look like under a microscope. This is also why the beer is called Corona, because of the crown that is on their logo. So although they have a similar name, the only similarity is the crown.
So what is a virus?
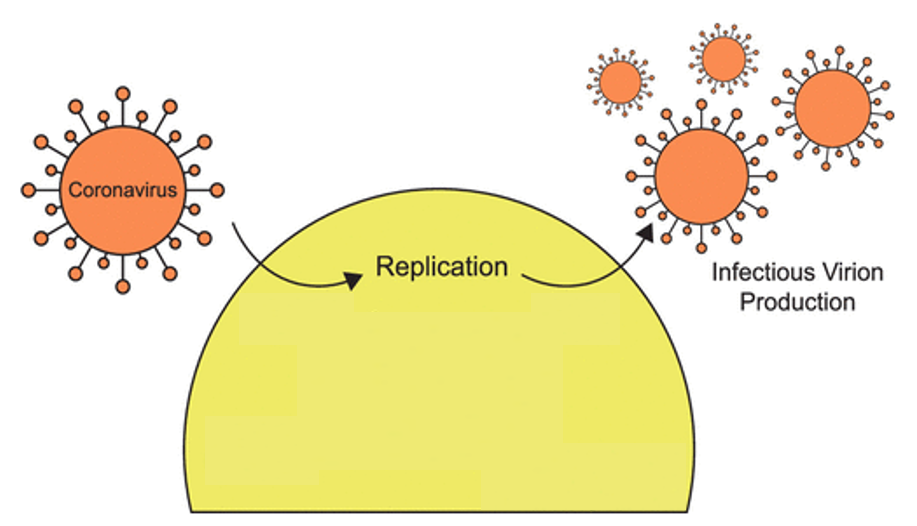
Since COVID-19 comes from a virus, we must not forget what viruses are, and what they can do. A virus is a submicroscopic and infectious particle made up of proteins and (DNA or RNA) that cannot reproduce on its own. The life cycle of viruses involves entering an organism and hijacking the host’s cellular machinery to reproduce. Newly reproduced copies of a virus burst the host cell to release the newly made copies. Some viruses are zoonotic, meaning that they can be transmitted from animals to humans through close contact. COVID-19 disease is a zoonotic virus, one that is transmitted from bats to humans.
COVID-19 Virus Has Some Relative
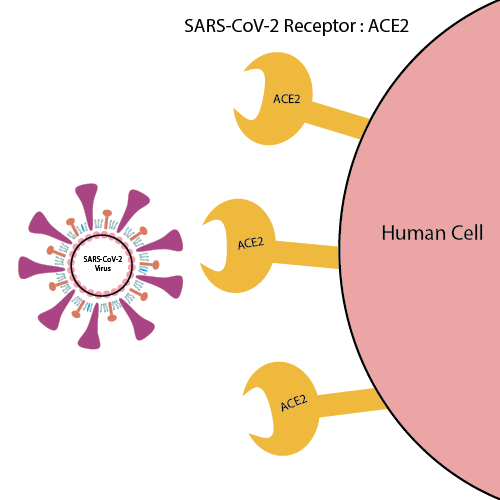 SARS-CoV-2 is just one member of the Coronavirus (CoVs) family, which also includes the MERS-COV and SARS diseases. Like the COVID-19 virus, all CoVs have the feature of surrounding spikes, which play an important role in how they bind to cells for replication. CoVs are RNA viruses with large genomes that encode for four major structural proteins – the spike protein (S), the membrane protein, the envelope protein, and the nucleocapsid protein. One way by which this family of viruses differs is by their receptor binding domain. A receptor binding domain is part of the virus on the spike protein that binds to the cell’s receptor and is known to play a key part in cell entry.
SARS-CoV-2 is just one member of the Coronavirus (CoVs) family, which also includes the MERS-COV and SARS diseases. Like the COVID-19 virus, all CoVs have the feature of surrounding spikes, which play an important role in how they bind to cells for replication. CoVs are RNA viruses with large genomes that encode for four major structural proteins – the spike protein (S), the membrane protein, the envelope protein, and the nucleocapsid protein. One way by which this family of viruses differs is by their receptor binding domain. A receptor binding domain is part of the virus on the spike protein that binds to the cell’s receptor and is known to play a key part in cell entry.
The Coronavirus Factory – Cells
The S protein of CoVs is highly responsible for starting the virus’s replication process. There are receptors outside of human cells called ACE2 receptors that are recognized by the S protein. The S protein binds to ACE2 and then is allowed to enter the cell. The cell then becomes a factory for CoVs. Coronavirus uses the cell’s machinery to make more copies of itself, and bursts it open to release the new copies.
 Infected by a virus? How does Your Body Prepare To Win The War?
Infected by a virus? How does Your Body Prepare To Win The War?
When a virus enters your body, an army of immune cell soldiers are commanded to infiltrate viruses to win the war against them. As part of killing the virus, your immune system makes proteins called antibodies that are designed to readily combat the virus if it tries to invade your body again. However, a virus can mutate into new strains (new varieties). If mutations are significant enough, new antibodies are needed because they don’t recognize the mutated form. This principle applies to the seasonal flu and is the reason why we get annual flu shots. Vaccines are designed according to differences in virulent flu strains that arise every year.
Although they are only slightly different, new strains of COVID-19 recently evolved in the UK, South Africa, and Brazil. Therefore, regardless if you previously had COVID-19, it is still a good idea to get vaccinated because your previous antibodies might not be protective.
Viruses and accustomed antibodies
COVID-19 and its World-Wide Debut
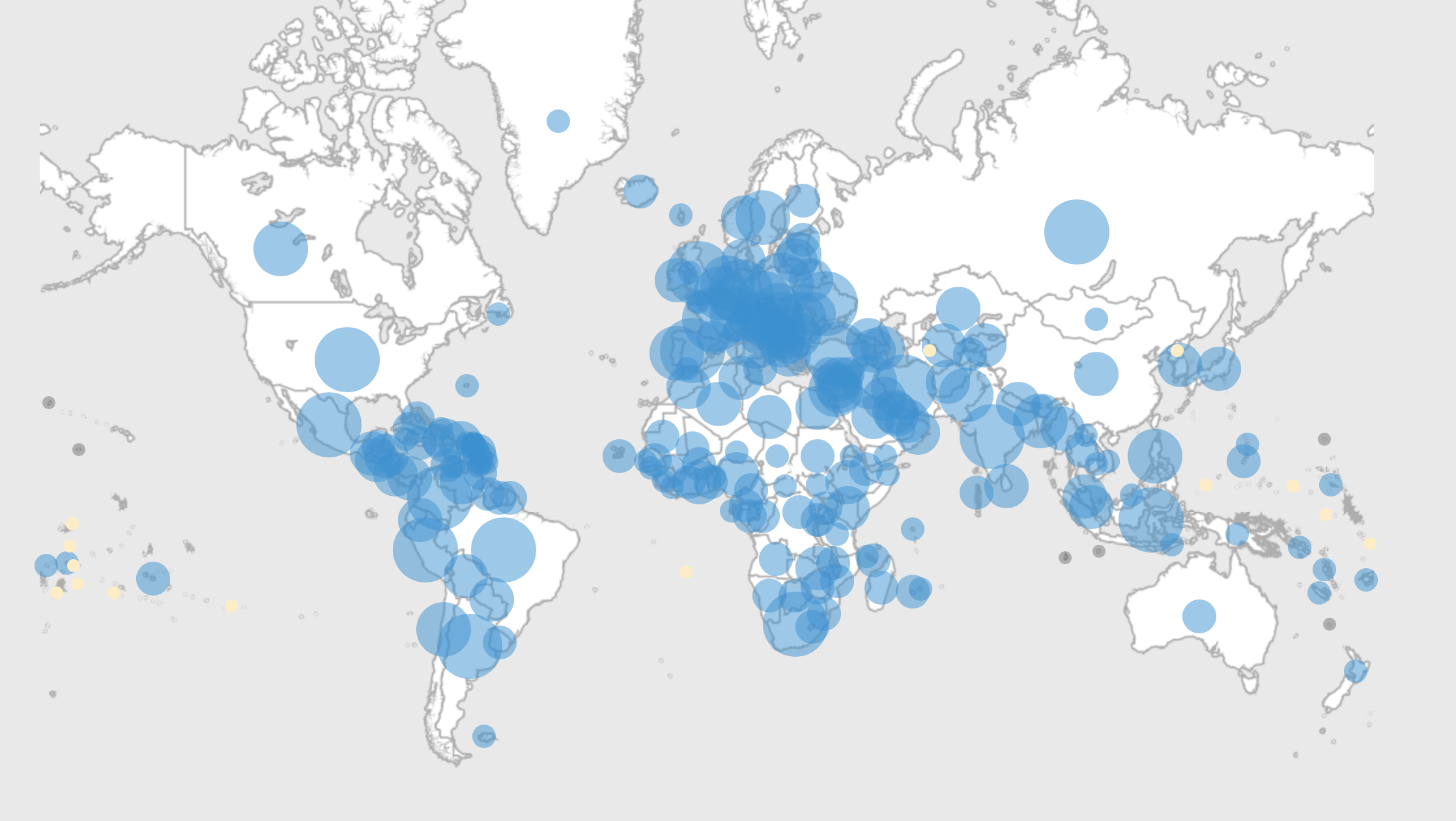
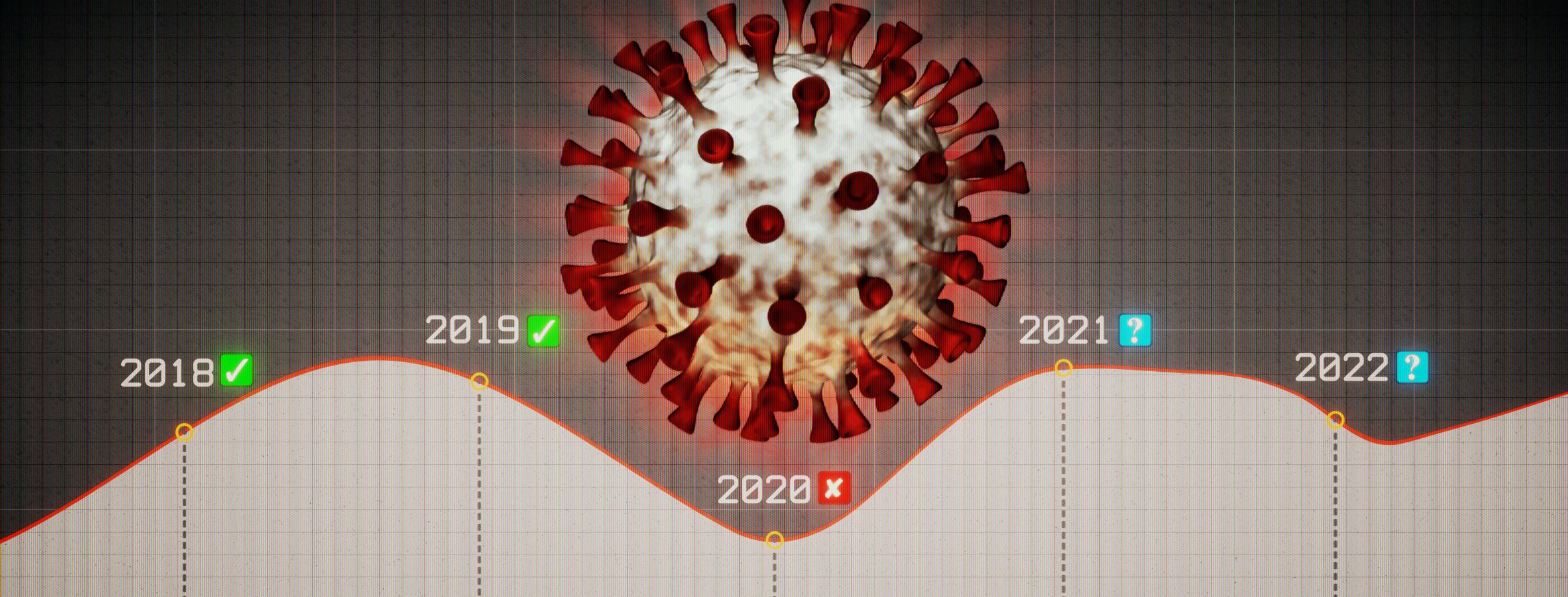
COVID-19 became a pandemic when it spread across the world in 2019. Its agenda is to continuously reproduce anywhere possible, and unfortunately on our behalf has achieved its goals. Circulation of the virus was first reported in Wuhan, China. 41 cases were reported to the WHO with an origin point of the Hunan seafood wholesale market, otherwise known as a “wet market.” Following this, cases continued to surge in China, and the WHO instituted a global public-health emergency. The first case of COVID-19 reported outside of China was in Thailand, on January 20th, 2020. Large upticks in cases began to take place in Italy and then New York City and soon the virus spread throughout America, Iran, and most of the rest of the world. On March 11th, 2020 the WHO officially declared COVID-19 a pandemic. As the pandemic continued, it was reported on November 9th, 2020 that cases around the world reached fifty million. Although cases are still arising, we can eradicate this virus by working globally while following precautionary measures.
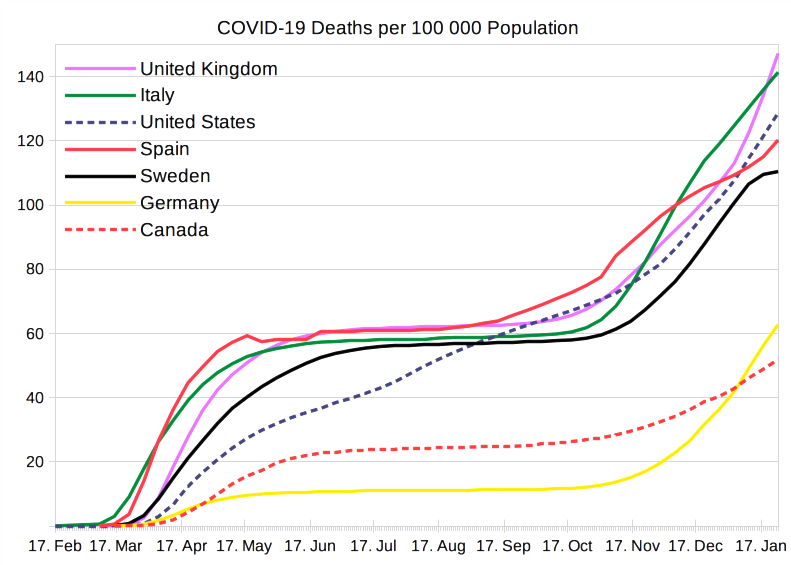
This figure shows the continuously growing number of COVID-19 Deaths in several countries. (From 02/2020)
COVID-19’s brutality is quantifiable in terms of cases and deaths. Yet the impact it will leave on us as species is still very much being determined. This sudden change is simultaneously transformative and terrifying, not only for those afflicted, but for how we deal with diseases as a species. In 2020 and into this new year, the world has endured a constant battle with COVID-19. Throughout, physicians and researchers have been able to document and alleviate certain aspects of the morbidities associated with this disease at a rapid pace. Their diligence, and the sacrifices made by their countless patients, have brought to light the clinical presentation, associated risk factors, as well as the prospective long-term effects of COVID-19 infection.
Expectations
As with many diseases, the suffering caused by COVID-19 can be physical, psychological, or some combination of the two, ultimately determined by what your prior ailments have predisposed you to. When considering how you might fare against COVID-19 in the near term it’s important to grasp the clinical spectrum of the disease. Generally, the clinical spectrum of SARS-CoV-2 infection adheres to five categories of illness severity. These categories are (1) asymptomatic, (2) mild illness, (3) moderate illness, (4) severe illness, and (5) critical illness. Asymptomatic patients will test positive using a virologic test, but have no associated symptoms. Those with mild illness may experience a multitude of symptoms (fever, cough, sore throat, malaise, headache, muscle pain, nausea, vomiting, diarrhea, loss of smell/taste) but are unlikely to develop loss of oxygen saturation if their disease state stays stable. Individuals afflicted with a moderate or severe diagnosis will experience the onset of acute respiratory distress syndrome and will have difficulties breathing due to damage and inflammation within their pulmonary system. If these symptoms progress a critical diagnosis can manifest, and these patients will suffer from hyper inflammation causing multiple organ failure, super infection, and further decline that will lead to intubation.
Exacerbations
Co-morbidities like obesity, and heart disease increase a person’s risk of developing severe COVID-19 as well as the complications that come with it. As COVID-19 has now swelled to overtake both heart disease and cancer as the leading cause of death in America, we should start to wonder about our overall health as a nation, and how we can address this issue not only in the clinic but prophylactically. It is estimated that 80% of heart disease can be addressed and prevented before the onset of serious disease, and the deaths of 30-50% of those diagnosed with cancer can be mitigated through the avoidance of key risk factors.
The reality of these statistics speaks volumes both about the availability of prophylactic care, and the implementation of such strategies in the daily lives of the people who are at risk for disease. The same is true for many of the aforementioned risk factors associated with COVID-19: implementation of preventative care can help at-risk individuals manage their conditions. However, there are certain predetermined factors such as our biological clock or predispositions such as genetic conditions that are inevitable when considering how we can best protect ourselves against disease. Considering the vulnerability of those around us, it’s imperative to not only mount our own defense against this virus but implore everyone to consider the fragile mortality of others.
End In Sight ?
The lasting effects of COVID-19 infection are still very much being determined. The recovery rate of those who are afflicted with a mild version of the disease generally trends higher; about 70% of those will return to their normal health within a short time frame. However, those suffering with more severe diagnoses will struggle to retain their previous health status without accruing new conditions or exacerbating previous ones. Generally, it is understood that the current lasting effects of COVID-19 infection present as somatic conditions such as acute organ damage, hyper inflammation, lasting infection, and decreased vital capacity. In addition, psychosomatic disorders can also manifest themselves during or after recovery, where the highest frequency diagnoses are anxiety disorder, insomnia, general mood disorders, and dementia. Whether these diagnoses are a manifestation of the virus, or exacerbations of previous psychiatric sequela remains to be determined by the scientific community. However, an incredible amount of work has gone into characterizing and documenting everything we can from this experience.
History repeats itself: COVID-19’s opportunity to become zoonotic
The novel coronavirus and the SARS outbreak in 2003 have a lot in common. Both originated under similar conditions and both are part of the coronavirus family. However, COVID-19’s death and infection rates have skyrocketed past SARS’ numbers. Interestingly, in 2017 epidemiologists from the WHO and a world renowned immunologist, Dr. Anthony Fauci, anticipated the emergence of new coronaviruses from the initial SARS outbreak in. In both SARS and COVID-19, the original hosts were said to be bats. Those bats infected other animals and ultimately transmitted the disease to humans making it zoonotic. Both SARS and COVID-19 had the ideal opportunity to become zoonotic.
In zoonotic infections, successful replication of viral pathogens from animals to humans is a very intricate process. The transmission of a pathogen to a host cell is not something that happens spontaneously. These interactions co-evolved over hundreds of years to make viruses replicable between various hosts. Determining the natural host of COVID-19 is crucial to preventing the transmission of disease and possibly inhibiting the next pandemic.
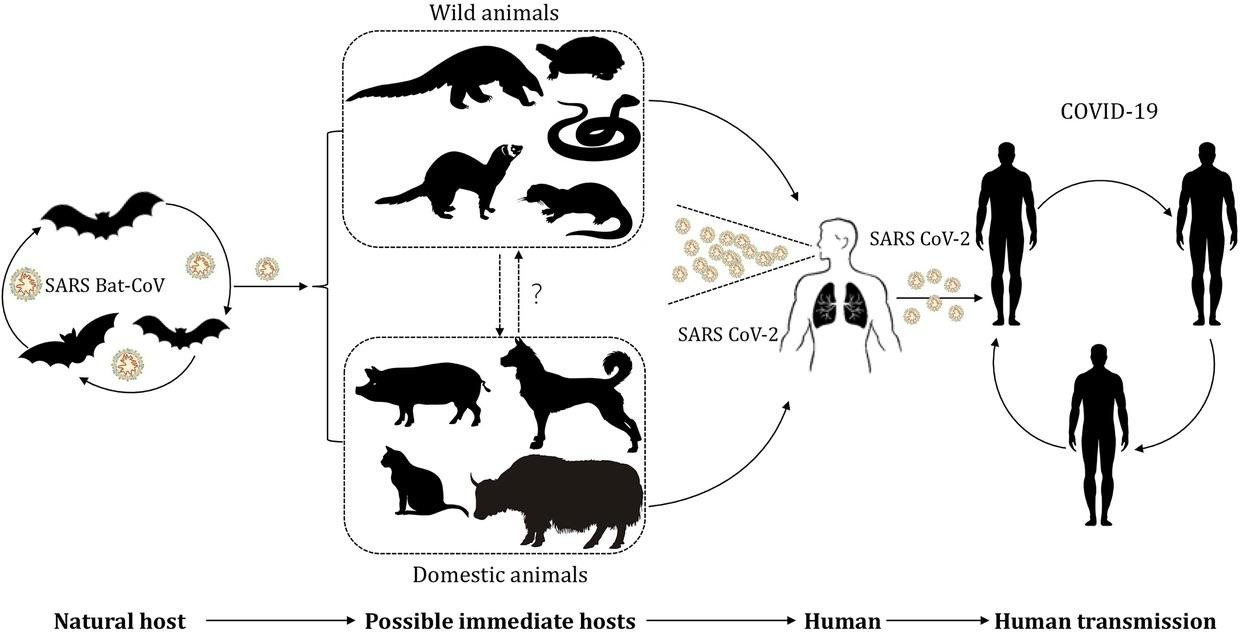
This image depicts the potential transmission of SARS-CoV-2 between different hosts and humans. Wet Markets provide the environment for this interaction to occur.
A wet market in Wuhan, China, where COVID-19 allegedly passed from bats to humans, has sparked conversation as to how viruses are given the opportunity to become zoonotic. Since the start of the pandemic and the mounting death toll, the markets have been put under the spotlight. Scientists from around the world teamed up to determine the intermediate host of this virus. Using various different analytical methods, researchers were able to come up with supporting evidence as well as opposed reasoning to determine how exactly the virus was able to transfer from animal to animal, ultimately making it zoonotic.
A Batty Virus
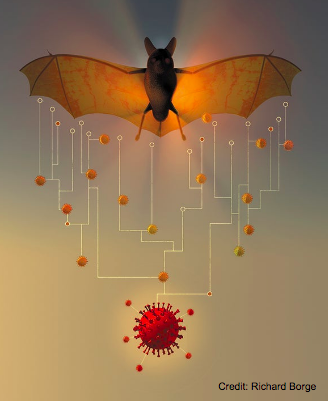 So how exactly did the scientists find out that the virus that led to the 2019 outbreak was a bat coronavirus? It’s known to the scientific community that SARS-CoV is mainly found in bats. Bats are also known to be natural reservoirs of many other viruses including rabies, ebola, and a wide range of SARS-like coronaviruses. A study was published in 2005 after the SARS outbreak which opened up research into bats and coronaviruses. Decades of intensive research of isolating and studying the genome of SARS-CoV had already confirmed the presence of SARS-CoV in bats. So with this previous discovery of bat SARS-related coronaviruses and comparative genome study, scientists were quickly able to confirm that the novel virus was not a lab manipulated virus. In fact, phylogenetic tree analysis which is used by scientists to study the evolutionary history and origin of different viruses, confirmed that the novel virus was 96% similar to a bat coronavirus at the whole genome level.
So how exactly did the scientists find out that the virus that led to the 2019 outbreak was a bat coronavirus? It’s known to the scientific community that SARS-CoV is mainly found in bats. Bats are also known to be natural reservoirs of many other viruses including rabies, ebola, and a wide range of SARS-like coronaviruses. A study was published in 2005 after the SARS outbreak which opened up research into bats and coronaviruses. Decades of intensive research of isolating and studying the genome of SARS-CoV had already confirmed the presence of SARS-CoV in bats. So with this previous discovery of bat SARS-related coronaviruses and comparative genome study, scientists were quickly able to confirm that the novel virus was not a lab manipulated virus. In fact, phylogenetic tree analysis which is used by scientists to study the evolutionary history and origin of different viruses, confirmed that the novel virus was 96% similar to a bat coronavirus at the whole genome level.
So, what makes bats so unique in hosting viruses? Some studies suggest that these flying mammals have high energy demands for flight which may lead to biological mechanisms of dampening which essentially means that the cells do not start an immune response to the virus. This limits any infection caused by coronaviruses. While scientists are still trying to understand the basic biology of bats, studies suggest that millions of years of evolution gave bats a very high tolerance for viral infection.
How did the virus to jump from bats to humans?
Scientists are trying to figure out how this virus jumped from bats to humans. A strong possibility is what’s called “recombination” or when genetic information is exchanged between two similar or identical molecules of the virus genome. They predicted that there could possibly be a recombination event between the bat coronavirus and another coronavirus. In a study done in Beijing, researchers analyzed 272 genomic sequences of coronaviruses from different geographic locations. They found that a pattern of genes utilized by SARS-CoV2 –– also known as codon usage pattern –– resembled that of snakes from China. This was interesting to learn because snakes were also sold at the Hunan market! While the natural reservoir of this virus is confirmed to be bats, the intermediate hosts responsible for transmission and evolvement remain unclear.
Thinking Ahead…
With the average development time for vaccines being 10-15 years, and with the previous quickest development time being four years for the Mumps vaccine, it was within reason to question the proposed development timeline of the COVID vaccine. The COVID vaccine was ready for distribution within a year due to the infusion of massive amounts of resources as well as advancements in medical technology. The U.S. Department of Health & Human Services launched a program they referred to as Operation Warp Speed in which billions of dollars were devoted to the sole purpose of COVID inoculation. Also, bearing in mind that the Mumps vaccine started being developed in 1967, the technological and medical progress accomplished up to the year 2020 played a tremendous role in the vaccine’s development. With the depth of analysis performed on topics such as mRNA along with the research that was conducted on SARS-CoV and MERS-CoV, it makes more sense as to how the vaccine was developed so quickly.
With everything considered, our fight against all pandemics that have come in the past, are occurring in the present, or will come to pass in the future will be a long and arduous process. Through scientific literacy, and the deployment of revolutionary technology our fight against disease can distill down into the choices we make. Choosing to advocate for the vaccine, making the decision to explain why treatments are effective, and calmly picking apart the apprehensiveness that manifests from the unknown, can be our greatest strengths as we face the ever-evolving threats to humanity.
Further Reading
Pandemics: Through the Looking Glass
A distinct name is needed for the new coronavirus
A together to Fight COVID-19
History of Smallpox
Visualizing the History of Pandemics
History of the 1918 Flu Pandemic
COVID-19 Virus Has Some Relatives
Cell entry mechanisms of SARS-CoV-2
COVID-19 deaths per 100,000 population
CDC: Precautionary Measures for COVID-19
Information about COVID-19 Vaccines
CDC: Understanding and Explaining COVID-19 Viral Vector COVID-19 Vaccines
Quotes of Madam Curie
A Batty Virus
Cross‐species transmission of the newly identified coronavirus
Lessons from the host defenses of bats, a unique viral reservoir
Genomic characterization and epidemiology of 2019 Novel Coronavirus
Insights into the origin of SARS coronavirus
SARS-like coronavirus and the ACE2 receptor
SARS coronavirus-like virus in Chinese horseshoe bats
History repeats itself: COVID-19’s opportunity to become zoonotic
Dr. Fauci warning the world about a potential outbreak stemming from wet markets
Determining the intermediate hosts- How scientists went about discovering the transmission pathway
Mumps Vaccine: How long do vaccines take to develop
Operation Warp Speed, efforts in producing the corona virus vaccine in under a year
Expectations, Exacerbations, & is the End in Sight?
COVID-19 Rising to Become the Leading Cause of Death in America
CDC Prevention Programs for Cardiac Disease
WHO’s Health Topics: The Major Risk Factors for Cancer
CDC : Major Risk Factors for COVID-19
Why does COVID-19 disproportionately affect older people ?
mRNA vaccine Efficacy
Clinical spectrum of SARS-CoV-2 Infection
MAYO Clinic: Long-Term Effects of SARS-CoV-2 Infection
The Lancet: Psychiatric connection to COVID-19
SHARE