The New Metrics of Functional Aging
Guest

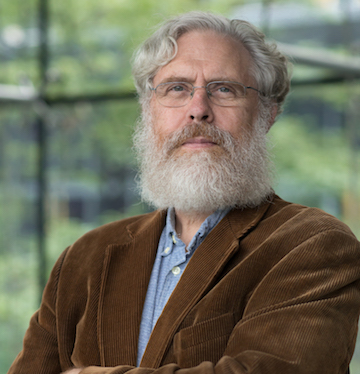
Jamie Justice, PhD
Executive Vice President of the Health Domain at XPRIZE Foundation, and Adjunct Professor in Internal Medicine Section on Gerontology and Geriatric Medicine, and Sticht Center on Healthy Aging and Alzheimer’s Prevention at Wake Forest University School of Medicine (WFUSM)
Jamie is the Executive Vice President of the Health Domain at XPRIZE Foundation, and Adjunct Professor in Internal Medicine Section on Gerontology and Geriatric Medicine, and Sticht Center on Healthy Aging and Alzheimer’s Prevention at Wake Forest University School of Medicine (WFUSM). She is dedicated to Geroscience research that advances the hypothesis that by targeting the basic biology of aging the incidence of multiple age-related diseases can be delayed or prevented.
TRANSCRIPT
Brianna Stubbs:
This episode is presented by Ashton Thomas Private Wealth, guiding families and institutions with clarity today and strength that endures for generations.
Jamie Justice:
We have actually already changed our population lifespan. We’ve done it through public health measures and modern medicine. So over the last 100 years, we’ve extended our human lifespan by around 30 years. And that’s pretty profound. That’s a lot. But what we’ve recognized is that the real thing we want to solve is autonomy, independence, and function.
Eric Verdin:
Aging is evolving. No longer are we subject to forces beyond our understanding and control. We have charted the landscape and explored the frontiers of aging.
Brianna Stubbs:
What was science fiction is close to becoming reality, restoring sight, repairing tissues, reviving cells, organs, and maybe even our minds.
Eric Verdin:
I’m Eric Verdin , CEO of the Buck Institute.
Brianna Stubbs:
And I’m Brianna Stubbs, a scientist here at The Buck.
Eric Verdin:
On this podcast, we dive deep into cheriscience, studying the intersection of aging and disease with some of the brightest scientific stars on the planet. Join us because we’re not getting any younger yet.
Read more close
Brianna Stubbs:
How’s it going, Eric?
Eric Verdin:
It’s going well. How are you?
Brianna Stubbs:
I’m doing well. I’m doing well. I just had an awesome non-running conversation with Jamie Justice, who’s uh, as you know, executive director of X Prize Health Span. She and I are longtime running buddies. We’re often having pre-sunrise conversations, pre-sunrise pre-coffee conversations about all things science. But we we sat down, had a really great conversation about her work and um you know what she’s doing, trying taking biomarkers and clinical outcomes into you know, making this moonshot prize to hopefully invigorate the aging field.
Eric Verdin:
Jamie is great. And you know, when I heard that uh Peter Diamandis had recruited her uh to uh help him run the X Prize for health span, I thought it could not have been a better person in the field.
Brianna Stubbs:
She’s so high energy and also has participated in some of the earliest uh kind of consensus discussions about like what does successfully uh reversing the biomarkers of ages aging look like. Um yeah, I think it couldn’t be a better person to be a spokesperson and a visionary of a this audacious goal.
Eric Verdin:
She also I think uh uh has the rigor that is really going to be critical in making the X-PRIZE a you know a benchmark that people will accept from a clinical standpoint. So you know she’d been running, she wasn’t involved in the TAME trial. And uh so I think all of this, her experience running uh real clinical trials is going to be critical in in establishing the X-PRIZE as a as a true benchmark for a field.
Brianna Stubbs:
I’m not sure whether I’m envious of her job or not, because picking between the hundreds of applications that they get, sifting through like the real uh very high quality applications and you know, ranging through to like the more crazy applications must be um a very difficult but interesting task. So um I’m excited to see where the prize ends up in the next five or ten years. We talk about all of this and more. Um so I hope you enjoy listening.
Eric Verdin:
I can’t wait to listen.
Brianna Stubbs:
Thank you so much for taking time to chat today. Um I know that you have a very, very busy schedule with your role with the X Prize, so we really appreciate the time and thank you for for making time to join us today.
Jamie Justice:
No, Brianna, it’s always my pleasure. Uh I love visiting the buck. I love hanging out, um, and I love all the uh all the collaborations that we’ve had over the years. So it is my pleasure to be here. There are a few things I’d rather do.
Brianna Stubbs:
You and I have spent a lot of time chatting, um out running in the mornings and had a lot of really good science conversations and also getting in our daily dose of uh longevity medicine just by being out and enjoying the trails. So um hopefully we’ll give people an insight into the kind of conversations that we have halfway up a mountain, first thing in the morning before a science meeting.
Jamie Justice:
Of course. Yeah, yeah. It’s amazing that we actually have as much conversation as we do before coffee. So one of the things that only can only be done running.
Brianna Stubbs:
So um I want to start by talking about um your kind of like scientific journey. Um you were previously in academia and and now in the X Prize. So that’s a pretty big change. And what what triggered that change and why do you think that’s such an important change to be happening right now for yourself?
Jamie Justice:
So it was a massive shift. This was not something that I went out and interviewed for. It’s not a job that I sought. Uh, in fact, I got a call that I thought I was being asked to be on an advisory board. I had never even heard of XPRISE Foundation and knew very little about it other than they had raised close to at that point $100 million to run a prize on HealthSpan. So to do work that was very much aligned with what I was already working on as a scientist. And so through my career, I had worked in a faculty exchange program through the GERScience education and training network, then co-supported by both the National Institute on Aging and American Federation for Aging Research, where I had an opportunity to work with key scientific uh leaders. And so we worked on ideas on, you know, how would you set up a framework to advance and accelerate preclinical to clinical testing, not for a disease doing direct development, but actually for aging. And that this was really relatively unexplored, there was no regulatory standards, and the field was fairly open. And so we tried to set up some of the first standards around that and had worked on it for several years, but it’s really difficult to incentivize a field to move in any one direction, is that there really does need to be some kind of an incentive or challenge for people to go after it in order to make change. Um, and that we had tried major initiatives like the TAME trial targeting aging with Metformin to create a regulatory pathway. We put out different special issues and series of papers. Um, the initial gyroscience network turned into a uh a larger gyroscience network, translational gyroscience network. We were at a spot where we were re-trying to reconceptualize if we were to rebuild the TAME trial, what would it look like? We’re like, okay, what else could the translational geroscience network be? What are some of the bigger approaches that could be done? Um, had uh a couple of active prizes and projects around um muscle and mobility and aging, and also thinking of new trials and how to combine um different drug trials with exercise or lifestyle. And throughout this entire time, I’d been really solution agnostic. It was really focused on how do you build the collaborative, how do you build endpoints, what biomarkers do you use, how do you vet them, how do you validate? Um, and you know, doing this sort of a piecemeal and trying to build collaborations, but collaborations are difficult without giving them use cases or something to chase. And so when XPRIZE approached me, I saw the potential. And so I could build all of the things that I had built on before. So going from animal models to early stage clinical trials, early stage trials to phase three, how do you interface with regulatory officials? How do you build consensus networks and collaboratives? We had a chance to do it in a way that was much bigger and more broad. And so, you know, again, don’t care if it’s a lifestyle intervention, a drug, a repurposed agent, a novel biologic, or any combination. And just have people have a chance to enter the competition, form collaborations, merge teams, merge ideas, and actually create the proof of concept that we need to actually show that aging is a tractable uh target for drug or therapeutic development. And I think that’s really the key that we’ve all been trying to build through not one pathway but multiple so that we can actually create change.
Brianna Stubbs:
I’ve heard our colleague and friend near Basley talk about like there is a drug, likely a drug on the market right now, which is a geroscience-based drug that targets hallmarks of aging. But when those trials are done by pharmaceutical companies, they don’t collect or share the data that would allow us to really um track that, plus everything that we’ve talked about so far around just consensus building about what that would look like. But we’re now building the framework that will allow us to say, well, what’s the next generation and what what treatment is kind of next? So in terms of what’s on the market and maybe things that are more like, you know, five years out, what what do you think might be the first um anti-aging drug that we already have? And what have you seen, especially with your seat on the X Prize? You must be seeing some things and you’re like, I really can’t wait to see where this is in five years’ time.
Jamie Justice:
Yeah, so I have to be a little bit careful. So again, I I love all of my children equally. So of course. I do. So I sit um as executive director, is that I’ve had a chance for those who haven’t had a chance to to check it out and are maybe just listening into this podcast for the first time. Um, you know, in 2023, we launched the prize. We invited uh folks, scientific um and um scientific contributors, advisors, and others to help contribute to how if we if you had the perfect drug or approach, how would you measure it? So we had a first initial public comment period. We invited teams to then register for uh for the prize. And in order to win the prize, uh, you know, teams have to have a therapeutic or an approach of any kind that they can demonstrate in one year clinical trials that they can that agent, given as they are within whatever their approach is and protocols, a loner in combination, can improve muscle, cognitive, and immune function. And so it’s not one or the other. So again, this gets back to that sort of multifactorial, it’s not just one disease, it’s not just one thing, it’s many. And that for one-year trials, we knew we’d never see those clinical endpoints like TAME. You’re just not gonna see that in a year. You need a lot of years for that. Um, so for these, we wanted things that we thought we could show a change in and that would not just be delaying or preventing, but like we you have to show that your function improves. That’s a very tall order. And the magnitude of improvement, you have to be able to offset the equivalent of 10, 15, or up to 20 years of expected declines.
Brianna Stubbs:
Yeah, all of us sitting here at the buck when the prize was announced and you know, we saw what you had to do to win the prize, everyone sort of really um raised their eyebrows and you know, thought that’s a pretty tall order. And and as you said at the start, it’s like planting a flag that’s really out there and is really pulling everyone after it. And so I think that whenever, whenever I talk about my work um running translational clinical trials, I love to mention the X Prize because I think that it’s like a real sign that the moment is now, that there’s a lot of that that that this, you know, I like to say in it’s not science fiction anymore, it’s science fact that maybe within the next, within our lives, we’re gonna have something that could feasibly reverse aging. And it’s like the confluence of all of the work that you’ve done and the things that we’re doing now here at the Buck to translate um all of that biology into meaningful endpoints. Um, it feels it feels like a very timely moment to be having this very um big audacious goal.
Jamie Justice:
Yeah. And boy, it is audacious. I mean, when we are putting these together, for me, with the data that I’ve run and have looked at, is that I think that 10 years in any one of those systems is probably the maximum that we currently have. So again, do we have something on the shelf right now that could be the thing? It’s like, you know, I it, you know, I think maybe for prevention and attenuation of declines over lots of time, like sort of that tame trial model, um, sure. Do we have something that’s going to be able to show improvement within one year? Um, I think what we are asking people to do is beyond what’s on the shelf. And so this is going to require people to collaborate. If you take people who are over the age of 60 and you do an exercise intervention, there’s been some meta-analyses done that if you take people who’ve never really exercised or not much, and you do a really focused exercise intervention, is that you can take those people and you can improve their VO2 max anywhere from 10 to 20%. I think it’s right around 16 to 18%, sort of on average in that population. That’s about the percent declines over 10 years. And so you could do it, but that’s one measure in one system. And so the challenge is trying to find something that can equal that kind of exercise effect on VO2 max that also has effects on muscle power, that can also improve executive function and working memory and those things for cognition, and can also benefit your immune system so that you’re more resilient and less inflamed. And so, you know, it’s it’s going to be a really big challenge. And, you know, I think 10 years for me, I think is the maximum that we’ll see. Peter Diamantes, who is our founder and very fearless leader, um, as soon as I told him you could maybe see it in one system and one measure, he said, great, that’s the starting point. We push him to 20 years. And I was like, Peter, you’re crazy. We’re never going to see it. Um, and so, you know, so we have graded out the amount that will be awarded so that, you know, we really our judges are going to be very clear. They want to see somebody who can have effects across multiple systems. And it has to be an improvement, not just a slowing decline.
Brianna Stubbs:
I think it’s really interesting that the prize is called X Prize Health Span rather than perhaps X Prize lifespan. So can you, you know, um, for the listeners who don’t know, can you talk a little bit about those two concepts and kind of where they overlap and then where they diverge and why we why you think one might be more important than the other, or in in what context one might be more important than the other?
Jamie Justice:
Yeah, absolutely. Okay, so there’s I would say this is this is a layered discussion. So one part of it is public health, one part of it is scientific advancement, and the other part of it is practicality. So the first is when we’re testing any kind of a therapeutic or we’re looking at uh changes, whether they be genetic, dietary, um, you’re looking even cross species, you know, your uh your lifespan, that median lifespan metric or the maximum lifespan is of course the ultimate test in whether or not something works too on aging is that if it affects aging, it should affect your median or maximum lifespan. That’s some of the forethought. And certainly if you’re doing that in animals, which um in my postdoc work, we did test interventions and some of them we tested for lifespan effects. And so you’re, you know, these are these survival studies are there forever long. And that, you know, your primary endpoint in that case is I would say the toes test is that you walk into your population of animals and you’re you know the vivarian, the mice, and you do the toes test. Are their toes up or are they down? And are they alive or are they dead? Toes down is you know, the animals are alive, of course, unless they’re up crawling around in their cages and things. But you know, so ideally that would be uh the worms have a toes up, toes down? No, no, I think the worms would be excused from the toes test. And so um, you know, so that’s pretty definitive. You can adjudicate that, right? So it’s really easy to judge. Animal alive, yes, animal dead, you know, no, those are zeros and ones, very binary, you can quantify it. And that, you know, over time is that what is actually more important out of that is probably not just the median lifespan, but would actually be uh the slope. So if you’re looking at a population, is you you’re looking actually at your mortality risk, and that if you change that slope or your risk of death at any point across the lifespan, then that of course would be the ultimate definitive. That’s your your gumperts. And so for those that are in the field, that’s um he’s the British actuary that you know really unknowingly um created some one of the most profound equations that has driven biogerontology for, you know, over a century. Um and so that would be the ultimate is if you have an intervention or do something that you change the slope, so you change the relationship between your chronologic age and your risk of death, then you can say you’ve done something fundamental to change the rate at which that animal organism is aging. Um, okay, so translating that up, two things. One, when we think about human aging, we have actually already changed our population lifespan. We’ve done it through public health measures and uh, you know, in modern medicine. So over the last 100 years, we’ve extended our human lifespan, our expected uh life, it by uh around 30 years. And that’s pretty profound. So that’s a lot. Um, and that we have now the first generations of people that are living longer. Um, but what we’ve recognized is that perhaps that toes test when we’re thinking about the population level and we’re thinking about human aging might not be the actual gold standard.
Brianna Stubbs:
Well, I think that what we see a lot when we um have visitors here at the buck is that people don’t want to live longer if it means that their health is not going to be good, right? So we all care about being out on the golf course or hiking up a mountain or doing all of those things for as long as possible. That’s right.
Jamie Justice:
And I would say that sentiment’s getting even stronger. Um, so you know, certainly now we have, you know, whole generations of uh of baby boomers who are actively caring for aging parents and you know, thinking about the long-term consequences of our extended life. And, you know, is that a life I want to live? And, you know, maybe we should rethink what this looks like. Um, and so there’s very much that public and personal relationship that we have with our bodies and with our families and with our communities. And we at the population level have a lot of concerns now that we might have financial and economic incentives that are unfavorable. And so, you know, in countries that have a much older population, there are incredible gifts with that. Huge gifts of having an older population. Um, you know, our older adults tend to um tend to have greater, they’ve done measures of wisdom, you know, they are active right now, and uh the the older segments of various populations are the source of some of the greatest economic um benefits, right? So they’re staying in the workforce longer and contributing quite a lot. Um, they have great roles within communities and multi-generational family structures. And so, you know, there is enormous potential and benefit to having an aging population, but if that is co-occurring with a lot of disease and disability and loss of independence and loss of autonomy, uh, then that’s the situation I think that we all need new solutions to go after. And we don’t have a drug development model to approach that at all. Everything in our drug and treatment development is that we wait for diseases to appear and then we try to treat them. With aging, we don’t get one disease, you get any number of diseases, conditions, and disability that aren’t necessarily disease-bound, but they tend to be syndromic or multifactorial. And we what we’re looking at when we think about now in the translation of some of those things, it’s not just thinking about the toes test, but when we’re looking at human aging, the real thing we want to solve is autonomy, independence, and functionality.
Brianna Stubbs:
Is there anything on those panels you think that is actually helpful for people now, or do you think that the only good things we have are, you know, the special services like DNA methylation clocks where you kind of mail off to a special company? Do people have some information that’s helpful now?
Jamie Justice:
Yeah, I you know, and and the important part, right, again, all of those methylation-based clocks, those were based on those clinical things that you just mentioned. So, like a pheno age was built and trained. So you’re just taking one biologic sample and you’re training it on a host of other measures. You know, pheno age is looking at some function and disease characteristics, but it’s really primarily based on, you know, a set of nine clinical lab markers that you can just take those lab markers and plug them in and still get a bioscore that’s still really important without doing the methylation. And in some cases, when Morgan Levine developed that, you know, I remember some of her early work was showing that actually just those clinical markers were in some cases more predictive of mortality risk than the methylation clock that was trained on them. Um, but you know, so again, it it is a matter to be a little bit careful. Uh the grim age clock is one of those methylation-based clocks that it does seem to perform really remarkably well. And so it’s highly predictive. It does seem to change with some interventions and that there’s some good support behind it. There’s another clock that’s trained completely differently that’s looking at pace of aging, so your rate of age and how that changes. So it’s actually tuned to detect the change over time. And so that’s a slightly different metric, but again, it seems like it may be sensitive to some interventions like caloric restriction in humans. Um, so I mean, there is some work going on with the methylation side, and that those are developing. Really rapidly and becoming validated. But again, they’re validated against what? And they’re trained on what. So I mean, they’re just trained in each one of them, they’re just calibrated typically to some gold standard measure that often we already have in our clinical record anyway. But that they could be really useful if you just need a single blood test, a single test to do X thing that might be more predictive in the future than those existing tests. And I think that there’s been a lot of progress there. But I do love clinical labs. And I think when I think about biomarkers, I think about them in different camps, right? So we have um, you know, really just targeted biomarkers where we have these things called hallmarks or pillars of aging. These are biological processes that we know across animal models, that they are associated with chronologic age across species. Um, and that they, if you block them, um, or let’s just say first, let’s aggravate them, you do something to turn that measure up, whether it’s, you know, some epigenetic alteration or uh stem cell exhaustion or one of these other pillars, if you do something to aggravate them experimentally, animals live shorter. So the toast test again. And the these biologic processes that underlie that are also shown to be accelerated. Um, those same processes, if you block them or turn them down, whether genetically, pharmacologically, or other, animals live longer. And so there are measures of those hallmarks that could be used in a really targeted panel. And that, you know, and I’ve seen this done in trials, is you pick a few across them and you show that you’re having multiple biologic effects. And that I think that that is also still a very attractive way to go. It can be more difficult to interpret because if you have some markers go up and some markers go down, you’re still left with, right, just like that Asprey trial where you have physical function might benefit, but overall it really didn’t. And so you still have to have some kind of an algorithm or a thing that helps you interpret those signals. Um, and so those algorithms to interpret those signals, we can think about those in composite biomarkers. They could be made up of those really highly tuned targeted markers. They could be really classic things that you already have in your clinical panels. That could be insulin. It could be a couple of inflammatory markers. Um, it could be, um, I know, gosh, I I really love cystatin C. It’s a kidney marker, but it seems to do a little bit of everything. Um, there’s also red shell distribution with is one of my very favorites. Um, so anybody, I have a big soft spot for RDW. So it’s one of those that you can get from a complete blood panel for like two bucks. And you get this measure that’s been associated with mobility, VO2 max, mitochondrial function. Um, it changes with age. You’re the cell cell distribution with it, you know. Again, it is a it is a nice, very simple, very cheap marker that’s you know, highly associated with the function and predictive of outcomes.
Brianna Stubbs:
It’s it’s such an exciting time because we have more of these big data sets where we can take things that we have in every trial because it’s in a common blood panel like RDW, uh, red cell distribution width, that was the right acronym. Um, we can take things like that that we have. We are increasing the number of biomarkers that we can measure with multi-omic approaches, but now we also have access to more um AI-based machine learning that’s going to help us integrate all of those old data sets with all of the new data that we’re developing to hopefully sort of streamline selection of things associated with multiple functional domains. And it’s it’s kind of challenging to figure out now without um without all of the computer processing power to integrate all of the data.
Jamie Justice:
Yeah, no, agreed, agreed. As you know, it it requires lots of data in order to train those systems properly. Um, and you know, one part of it is actually making sure that we are collecting the right data and that it is being centralized and is open access. And so this is an again another really big challenge is that in many cases there is data out there, um, but it’s not well integrated and it’s not in a place or in a format that can be used by these larger models. Um and so that’s something that you know have heard tossed around as sort of dark data, is data that exists, but is really it’s hidden, um, and hidden for various reasons. Some of it is because, right, it might have been collected at a time or in a place where their human protections didn’t allow it to be shared or other. So, I mean, there can be good reasons for that. But I think as we’re becoming more savvy and we’re learning a lot more and making better use out of those large uh those the big data sets that are out there and making better computational uses, I think that those are only going to improve. Um, but we have to feed in the right data to them. And so that’s coming from clinics. I think we’ve seen a lot of clinics really begin to open up their data and share those through new models. And so clinics who are doing, you know, working with uh, you know, longevity medicine clinics or others that are actually doing really novel therapies and things that we’re talking about testing and trials is that they’re actively prescribing off label or administering. And so, I mean, that’s a huge opportunity for those uh clinics and groups to feed that data in so that we can actually get real uh real insights a lot earlier than waiting for large trials, which also have to happen on the regulatory side. And so, you know, just trying to think of ways to get out of that, you know, that’s my Spider-Man meme of everybody standing waiting and pointing at each other, you know, that there are chances to do that and make better use of the data that exists.
Brianna Stubbs:
I um I love that we started talking about you and me out running and you actually finished kind of coming towards the end here, finishing talking about the importance of VO2 Max exercise. Um, obviously, as you said, for physical muscle, physical function, exercise has been linked to improved cognitive health or as part of multi-domain um lifestyle interventions as well. And um I feel like through the podcast series, I can imagine my own personal bias as an athlete is gonna be to talk a lot about the importance of exercise. And I know you agree with me too. Yeah, I’m yeah, I’m on your soapbox. Exercise is outstanding. Yeah, every everyone should be doing a little bit more than they do now, unless you’re like me in training for an ultramarathon, in which case sometimes more isn’t always better.
Jamie Justice:
Yeah, I was gonna say, yeah, I think you and I have reached the threshold that more is not better. Um, yeah, I unfortunately, Brianna, I’m on the injured list again. Oh no, I’m sorry. I know it’s happened. So um, you know, and it just happened. So this has not been my year. I’ve had some hip injuries, and so I notice it when I stop running more than ever.
Brianna Stubbs:
Yeah.
Jamie Justice:
And so I’m still active. I still do other things, but you know, yeah, it’s uh it it does become a a lifestyle and it’s one that I do expect a lot of our teams to try to lean into how they consider exercise as part of their approach. And one thing I will also say for these trials is that, you know, we don’t, I don’t think it’ll be one by exercise alone. So for those that are out there and you think, you know, I’m gonna exercise and it will it will overcome all ills, and that will probably be all I need. Um, it is a part of a very critically important solution, but it is part. You know, I think their other lifestyle, we have one of our teams that’s leaning really deep into circadian rhythms, which would be awesome for your podcast. I’ll make that recommendation later. But looking at how you could re-time medications that are given for chronic disease management. And if you can put them on a circadian rhythm and pair those with other sort of lifestyle behaviors that follow that rhythmicity, is it you can create exponential effects on top of what you’re just given in your daily life? Um, and then there’s others that are looking at how you would use exercise combined with a drug to have some kind of additive or synergistic effect. And we also have evidence in the literature that that’s not always a one-to-one.
Brianna Stubbs:
Yeah.
Jamie Justice:
Right. And so there was a study that looked actually, and I love metformin. I mean, I worked on the chemtrail, huge, huge fan. But when they did this study and they did metformin given at the same time that a resistance exercise program was started, when those were timed together at six months, there were some of those protein signaling pathways in the muscle that weren’t better by doing metformin and exercise, is that they’re both something called mitohermetic. So they put pressure and stress on the mitochondria, and that more isn’t always better when you’re targeting the same system. And so there may actually be in some cases, and the metformin one, I don’t think it was detrimental. It’s just that you didn’t get an additive. Um, and so how that affects function later to be determined. Um, but I would say, you know, just the the folks that are out there thinking I’m gonna do everything, right? Is that I’m gonna take every drug and every nutraceutical and try every platform and I’m gonna do them all at the same time, is that that might not be the winning strategy. So, again, going back to those biomarkers, going back to those clinics, going back to having ways to make informed decisions that suit your body, it’s gonna be hugely important. And we’re not gonna unlock that by doing traditional trial design. And so, again, this is one of those other things that I was seeing and seeing and seeing as a scientist that when I saw XPRIZE, was like, okay, this is a chance to do something different, to push people out of this very rigid structure that we’ve been designing trials by. And it’s really not how humans function, it’s not how we take drugs, it’s not how we necessarily should even be testing them because it’s not how they’re given. So I don’t know, I’ll get off my soapbox now, but yeah, exercise part. Part.
Brianna Stubbs:
I’ve said said this earlier, I’ll say it again. I really feel like the field is at an inflection point. We’re able to test, we’re building consensus, able to test more things. We have a lot of candidates. And um, I just really appreciate having like colleagues like yourself in the field who did so much of that early groundwork to lay the lay the, you know, to lay the foundations for what we’re gonna hopefully see in the next five, 10, 15 years. And I guess like a last mini question, if if I have time, would be um the end of your career. So we’re not talking like 10 years, we’re talking 30 years time, 40 years time. You know, I hope that you’re I hope that you’re active in the field for a long time. But when when you finally sort of step back, how would you like to leave the field? Um, and where do you think it’ll be when you when when you look back at your career?
Jamie Justice:
Yeah, when I look back, what I would like to what I would like to be down for is clinical trial innovations um in aging. And I would like to be, you know, somebody who has at least helped unlock some of these conversations to build a collaborative community around science is it should not just be competitive and small labs working in isolation. Um, the other part that I hope to create a legacy is actually is bringing the public into our science. And so this is another thing that I know the buck is really well aligned to is that I think the days of us toiling in a lab and under with federal dollars and sort of keeping our science only fed by scientific communities, I think that’s for the dinosaurs. Is that, you know, when we’re working on science and building a science legacy, is that it needs to be public. And so that means bringing people in, bringing people along, you know, establishing new trainees, creating a public discourse in whatever way that is. Um and so uh I those are would say if I’m looking at the key legacies, that’s what they would be around.
Brianna Stubbs:
Yeah, and those are critically important things. And thank you so much for your commitment to those. And thanks again for taking time to talk with us today. We we appreciate you um and all the work that you’re doing.
Jamie Justice:
My pleasure. Always my pleasure.
Brianna Stubbs:
Thank you so much for listening. Please subscribe, share, and give us a five-star review on Apple, Spotify, or wherever you get your podcasts.
Eric Verdin:
We’re not getting any younger yet. It’s produced by Vital Mind Media. The Buck Institute’s very own Robin Snyder is the executive producer. Wellington Bowler is right next to us here directing the recordings, and the esteemed Sharif Ezzat weaves the show together for you.
Brianna Stubbs:
If you’re listening to this podcast, you know that there has never been a more exciting time in research on aging. Discoveries in the labs are moving into the clinic to help us all live better longer. The Buck Institute depends on the support of people like you to carry on our breakthrough research. Please visit us at BuckInstitute.org to learn more and to donate. This episode was sponsored by Ashton Thomas Private Wealth, where discipline shapes vision and vision builds legacy. Learn more at Ashton Thomas PW.com.
Speaker:
Investment advisory services are provided by Ashton Thomas’ Private Wealth at L C and Ashton Thomas Securities at LLC, SEC Registered Investment Advisors. Securities are offered through Ashton Thomas Securities LLC, a registered broker dealer and a member of FinRA CIPIC.